Published by Bupa's health information team, December 2007.
This factsheet is for men who have testicular cancer, or
anyone who would like information about it.
According to Cancer Research UK, each year about 1,800 men are
diagnosed with testicular cancer in the UK. It accounts for one to two percent
of all cancers in men. Most men with testicular cancer can be cured. It's most
likely to occur in young and middle-aged men
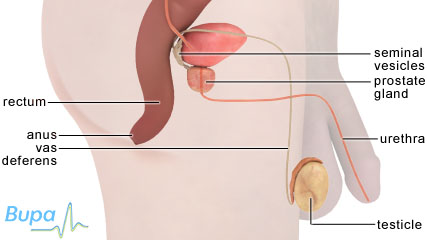
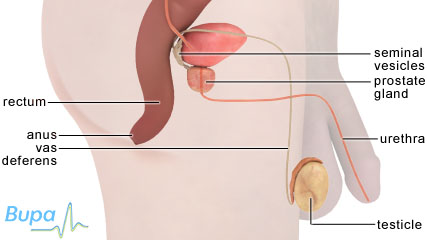
The testicles are located inside the scrotum, the loose bag of
skin that hangs below the penis. From the start of puberty, each testicle
produces sperm. The testicles also produce the hormone testosterone.
A testicular tumour is a lump created by the abnormal and
uncontrolled growth of cells. Testicular tumours can grow and sometimes spread
to other parts of your body (through the bloodstream or the lymph system).
Testicular cancer can also spread to the lymph nodes (part of the lymph system)
or form tumours in the lungs or other organs. The spread of cancer is called
metastasis.
There are two main types of testicular cancer: seminoma and
non-seminoma. Seminomas are made up of a single kind of testicular cell, while
non-seminomas (eg teratomas) are made up of more than one type of cell.
Very rarely, another type of cancer, called a lymphoma, can
occur in the testicles. This is cancer of the lymphatic tissue (tissue that
forms part of the immune system). Lymphoma is the most common type of testicular
cancer in men over 50.
The main symptom of testicular cancer is a lump, irregularity
or swelling in one testicle. Other symptoms that may be present include:
These symptoms don't always mean you have testicular cancer.
But you should see your doctor if you are concerned about your symptoms.
A few men with testicular cancer may experience lower back
pain, stomach pain or a cough as their first symptoms.
The causes of testicular cancer are unknown, but the number of
men who develop testicular cancer is increasing and research is being carried
out to find out why.
Men born with an undescended testicle (one that remains in the
abdominal cavity rather than descending into the scrotum) may be at greater risk
of developing testicular cancer.
Other factors that are thought to make testicular cancer more
likely include:
Having a vasectomy or injury to the testicles does not cause
testicular cancer.
Most lumps in the scrotum are not testicular cancer. However,
if you notice one or more of the symptoms above, you should see your GP or a
local sexual health clinic for advice. They will carry out a physical
examination to rule out any other conditions or infections that can cause
similar symptoms. Your GP may then refer you to a urologist - doctor
specialising in the urinary organs - at a local hospital. You may also need to
have an ultrasound scan so your doctor can examine your testicles.
If the ultrasound scan suggests cancer, a surgical procedure
called a biopsy will be carried out to confirm this, and to see what type of
cancer it is. This involves removing a small amount of the tumour and examining
it under a microscope. If the biopsy confirms that there is cancer, the doctor
will remove the affected part of your testicle.
Other tests may be carried out to see whether the cancer has
spread. These may include:
Assessing how far the cancer has spread is called staging. The
stages are:
The type of treatment used depends on the type of cancer and
how far it has spread. Chemotherapy and radiotherapy can temporarily lower your
fertility. As a precaution, many men store (cryopreserve) their sperm in a sperm
bank before treatment.
Surgical removal of the affected testicle (orchidectomy) is
the standard initial treatment for testicular cancer. If the cancer has spread
further, you may need to have chemotherapy first, so the removal of your
testicle will be delayed. You may wish to have an artificial testicle (an
implant or prosthesis) inserted into your scrotum - you can discuss this with
your doctor before the surgery. The removal of one testicle will not affect your
ability to have erections or father children.
After surgery, you will be referred to a team of specialists
and seen by an oncologist - a doctor specialising in cancer - to decide on the
best course of further treatment.
Early stage seminomas are treated with radiotherapy, or
sometimes chemotherapy (see Related topics). More advanced stages are treated
with radiotherapy, if the cancer is confined to a small area, or chemotherapy if
it's more spread out.
If you have an early stage non-seminoma, you probably won't
need treatment, but you will be monitored for any signs of the cancer coming
back (relapsing). This is because if testicular cancer does come back, there is
a good chance that it can be cured with chemotherapy. Chemotherapy can leave the
remains of tumours behind, and these may need to be surgically removed to make
sure the cancer doesn't come back.
After your treatment you will need to have follow-up
appointments so your doctors can see whether the cancer has come back. Depending
on the nature of your testicular cancer, your surgeon or oncologist will arrange
follow-up care.